A new study from the University of Bristol found that patients aged 50 to 70 who received a mechanical heart valve had better long-term survival than those who received a biological valve. The findings, published in the European Journal of Cardio-Thoracic Surgery, suggest that this age group’s increasing trend of using biological valves should be reconsidered.
“Our study has implications for decision-making in surgical heart valve replacements for patients between 50 and 70 years old,” said Professor Gianni Angelini, lead author and Director of the Bristol Heart Institute. “The evidence supporting better long-term survival in patients receiving a mechanical heart valve suggests the current trend favoring biological valves in this age bracket should be urgently reconsidered. The survival benefit is obvious in smaller-sized valves.”
Shifting Trends in Heart Valve Replacement
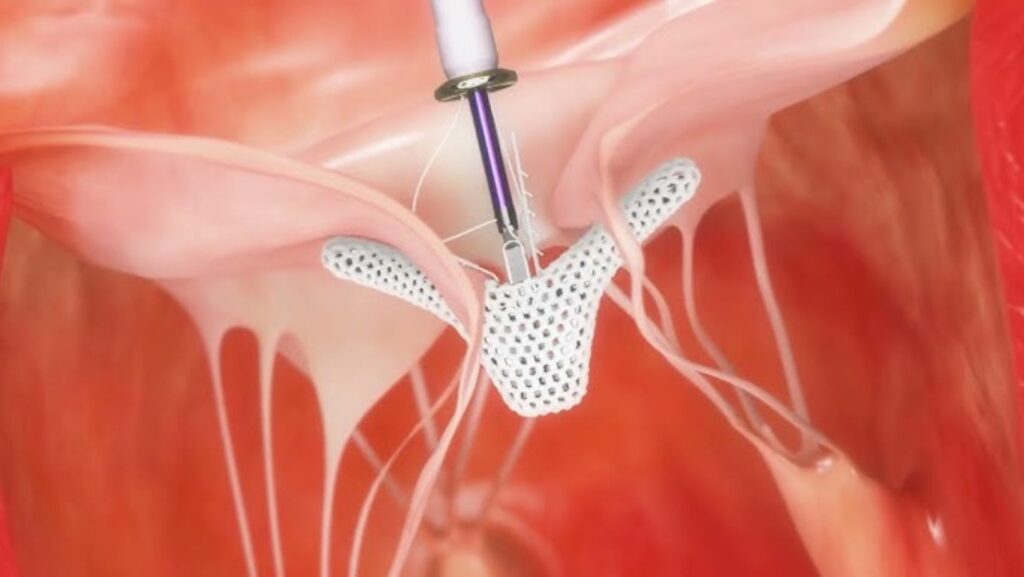
Over the past two decades, there has been a growing preference for biological valves (made from animal tissue) over mechanical valves (made from synthetic materials). While short-term survival rates are similar, long-term outcomes remain under debate.
Current guidelines recommend:
- Mechanical valves are more durable for patients under 50.
- Biological valves are available for patients over 65 or 70 since they do not require lifelong blood thinners.
- Patients aged 50 to 70 are left to decide with their doctors, as there is no clear guideline.
This study aimed to provide long-term survival data to help inform decision-making for this age group.
Study Findings: Mechanical Heart Valve Offer a Survival Advantage

Researchers analyzed 1,708 patients (61% male, average age 63) who underwent elective and urgent heart valve replacement at the Bristol Heart Institute between 1996 and 2023. Of these, 1,191 (69.7%) received a biological valve replacement.
Key findings include:
- No difference in short-term survival between mechanical and biological valves.
- Better long-term survival (up to 13 years) in patients with mechanical valves.
- Patients with smaller biological valves (19 mm) had the worst long-term survival.
- Patients with a 21 mm mechanical valve survived better than those with 19 mm or 21 mm biological valves.
The study also confirmed that severe patient-prosthesis mismatch (PPM)—when a valve is too small for the patient’s body—is a significant risk factor for poor long-term survival.
Implications for Surgical Decision-Making
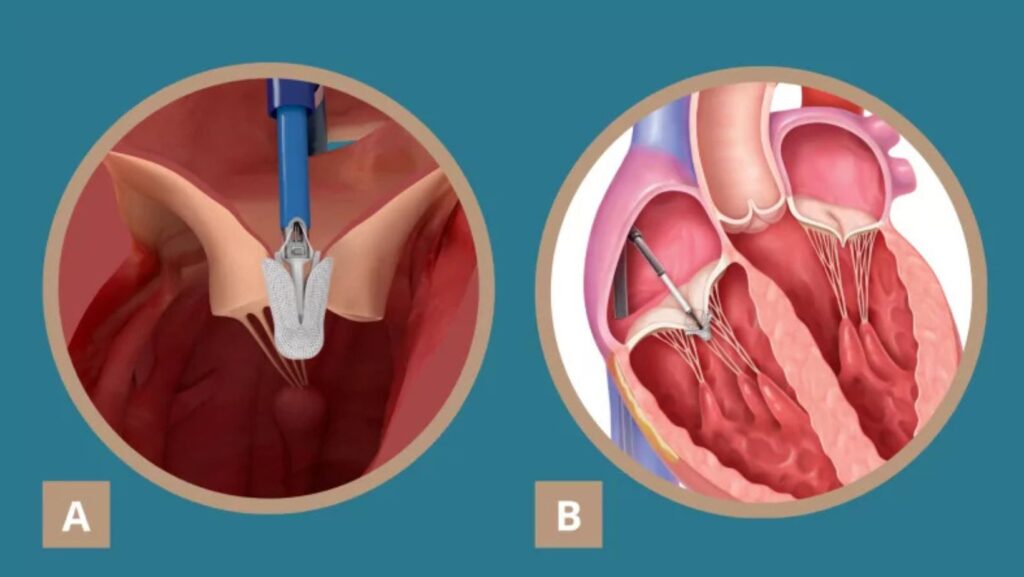
The research team recommends re-evaluating mechanical valve use in patients aged 50 to 70, especially in cases where smaller-sized valves are needed. While biological valves eliminate the need for long-term blood thinners, the survival advantage of mechanical valves may outweigh this benefit in many cases.
Limitations and Future Research

The study was based on retrospective data from a single institution, making it vulnerable to bias. Additionally:
- Echocardiographic data were not available, potentially underestimating structural valve failure rates.
- Re-interventions were only counted if performed at the Bristol Heart Institute, meaning some cases may have been missed.
- The cause of death (cardiovascular vs. non-cardiovascular) was not recorded.
Despite these limitations, the study provides essential long-term survival data that could influence future heart valve replacement guidelines and help patients make more informed decisions.
Reference: Jeremy Chan, Pradeep Narayan, Daniel P Fudulu, Tim Dong, Hunaid A Vohra, Gianni D Angelini. Long-term clinical outcomes in patients between the age of 50-70 years receiving biological versus mechanical aortic valve prostheses. European Journal of Cardio-Thoracic Surgery, 2025.

